Background
The burden of community-acquired pneumonia (CAP) ranks the first among all infectious diseases, especially in the elderly people, with higher morbidity and mortality, more comorbidities and complications, higher need for admission to intensive care unit (ICU) and rate of clinical failure (CF), and more medical expenses.1–5 Cardiovascular diseases (ischemic heart disease, stroke) are the world’s biggest killers, responsible for 27% of the world’s total deaths in 2019, according to the World Health Organization (WHO).6 The incidence of CAP and cardiovascular diseases significantly increases with advanced age.5,7 Previous study indicated that older patients hospitalized with pneumonia had fourfold increased risk of subsequent occurrence of acute cardiovascular events (CVEs) in the first 30 days after pneumonia.8 A clinical rule that stratifies the risk of cardiac complications in patients hospitalized for CAP revealed that older patients are at major risk of CVEs after pneumonia.9 A global systematic review and meta‐analysis of observational studies demonstrated that the overall rates of cardiac complications after CAP were 13.9%, and the rate of heart failure was 9.2%, arrhythmias 7.2%, acute coronary syndromes 4.5%, and stroke 1.7%.10 Meanwhile, the occurrence of CVEs complicated the course of hospitalization with CAP. Compared to CAP patients without CVEs, CAP patients with CVEs had higher rate of mechanical ventilation, more need to ICU admission, prolonged length of stay (LOS), higher rate of short-term and long-term mortality, and higher 30-day re-hospitalization.10–12 Therefore, the mutual interaction between these two diseases should arouse more attention of respiratory physicians and cardiologists.
Current studies mainly focus on the overall population of patients with CAP, yet rare data are for the certain elderly population.13 Accordingly, we performed a multicenter, retrospective study to evaluate the burden of CVEs during hospitalization and to explore the independent prognostic factors for the occurrence of CVEs and 30-day mortality in elderly patients with CAP.
Methods
Study Setting, Design and Participants
This study is a multicenter, retrospective research on hospitalized elderly patients with CAP from the CAP-China network. Data of patients aged 65 years or older were abstracted from 13 centers in seven cities in three provinces between January 1, 2014 and December 31, 2014 (details are made available in the study by Han et al4). The study was approved by the Human Subject Protection Program Institutional Review Board at China-Japan Friendship Hospital. Additional approval was obtained from the local institutional review board of each participating hospital. Patient consent was waived owing to the retrospective and observational study design.
Inclusion/Exclusion Criteria and CAP Definition
Inclusion criteria included (1) age ≥ 65 years; (2) one of the top five discharge diagnoses defined as CAP. Exclusion criteria included (1) hospital-acquired pneumonia; (2) active tuberculosis; (3) non-infectious diseases, such as pulmonary infarction, tumor or pulmonary edema; (4) acquired immune deficiency syndrome; (5) re-admission within 72 hours after discharge.
CAP was defined as follows: (1) community onset; (2) presence of new infiltrate on chest X-ray or computed tomography scan together with at least one of the following: (i) new or increased cough (productive, non-productive or with a change in sputum characteristics) with or without dyspnea, chest pain or hemoptysis, (ii) fever, (iii) rales and/or signs of consolidation, (iv) peripheral WBC counts >10,000 cells·mm−3 or <4000 cells·mm−3, with or without a left shift toward immature forms.
Immunocompromised patients referred to these with solid-organ or stem cell transplant or bone marrow transplantation within one year of admission, chemotherapy for hematological disease or solid-tumor malignancy within six months of admission or neutropenia <500 cells·m−3, chest radiation therapy within one month of admission, prescription with immunosuppressive therapy within three months of admission or splenectomy.
Data Collection
Details on admission such as demographic data, a series of clinical information, hematological data, evaluation of initial antimicrobial treatment, are also available in the study by Han et al.4
Clinical failure (CF) is divided into early (≤72 hours) CF and late (>72 hours) CF. The detailed definitions are available in the study by Han et al.3
Definition of CVEs
The CVEs considered during the hospitalization were defined as follows:
- Events related with cardiac diseases: ① congestive heart failure (CHF) (new onset heart failure, or worsening preexisting heart failure with typical signs and/or symptoms associated with elevation of brain natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP);②new onset arrhythmia, or worsening preexisting arrhythmia (multifocal atrial tachycardia, atrial fibrillation or flutter; ventricular tachycardia, flutter or fibrillation; new onset of high degree atrio-ventricular block (2nd and 3rd));③ acute myocardial infarction (AMI) with typical signs or symptoms associated with troponin level above the normal value (according to the reference range values of local laboratory) and/or ischemic electrocardiographic changes (new ST-T changes or new left bundle branch block).
- Events related with cerebrovascular diseases (CVDs): new onset of hemorrhagic or ischemic stroke or transient ischemic attack defined as clinical manifestations and was confirmed by computed tomography or magnetic resonance imaging.
- Events related with thromboembolic diseases: pulmonary embolism (PE) or deep venous thrombosis (DVT) was confirmed by clinical manifestations and by pulmonary artery angiography computed tomography or eco-Doppler ultrasound, respectively.
All the patients diagnosed with CVEs (International Classification of Diseases, tenth revision [ICD-10] codes (in the Additional file 1: Table S1)) were based on clinical manifestations, laboratory tests and consultation with specialists.
Statistical Analysis
According to the occurrence of CVEs during hospitalization, the patients were divided into CVEs group and non-CVEs group. Categorical variables are presented as frequencies or percentages, and continuous variables are presented as median (interquartile range, IQR). The χ2 test is used for categorical variables and the Mann–Whitney U-test for continuous variables.
Variables showing significant difference in univariate analysis (p<0.10) are included in multivariate logistic regression analysis model for the occurrence of any CVEs and 30-day mortality in elderly patients with CAP, and a stepwise forward model is used to select independent risk factor. The 95% confidence intervals (CIs) and level of significance are reported.
All data are analyzed with SPSS (version 20, IBM Corp., New York, USA); p<0.05 is considered statistically significant.
Results
Study Population and Clinical Characteristics
Excluding immunosuppressed patients, 2941 patients aged ≥ 65 years were finally analyzed. 13.7% (n=402) of elderly patients with CAP occurred CVEs during hospitalization. Among them, 80.3% (n=323) were with acute CHF, 25.9% (n=104) with arrhythmia, 8.2% (n=33) with AMI, 6.2% (n=25) with CVDs, 4.0% (n=16) with thromboembolic diseases (six with PE and 10 with DVT). 73.1% (n=294) of patients had any one of CVEs, 22.6% (n=91) had two types of CVEs, 4.2% (n=17) had three types of CVEs.
Clinical characteristics of patients with or without CVEs are provided in Table 1. Patients with CVEs during hospitalization were older, higher risk of aspiration, long-term bedridden confinement and more comorbidities, especially cardiovascular disease and CVDs. Compared with non-CVEs patients, the pneumonia severity in patients with CVEs was more severe, history of CAP in past one year and use of glucocorticoids during hospitalization were more common.
 |
Table 1 Comparison of Clinical Characteristics in Hospitalized Elderly CAP Patients with or without CVEs (n=2941) |
Clinical Manifestations, Laboratory and Radiologic Findings
Compared with non-CVEs patients, the rates of wheezing, cyanosis and lower extremity edema were more common in patients with CVEs, as well as unstable vital signs. Leukocytosis, hyperglycemia, azotemia, hyponatremia, hypoxemia, acidosis, hypoproteinemia, multilobe infiltration and pleural effusion were more prone to occur in patients with CVEs. During hospitalization, the incidence of related acute organ failure, diffuse intravascular coagulation (DIC) and gastrointestinal bleeding was notably different between the two groups (Table 2).
 |
Table 2 Comparison of Clinical Manifestations, Laboratory and Radiologic Findings in Hospitalized Elderly CAP Patients with or without CVEs (n=2941) |
Outcomes
Compared with non-CVEs patients, patients with CVEs during hospitalization were more prone to be admitted to ICU, administrated more guideline-discordant antibiotic therapy, higher rate of CF, and lower rate of clinical stability before discharge. The median LOS in patients with CVEs was 12 days, significantly longer than that (11 days) in non-CVEs patients (p=0.019). The in-hospital mortality and 30-day mortality were also significantly higher in CVEs patients than those in non-CVEs patients (p<0.001), 27.1% versus 2.0%, 30.3% versus 3.4% respectively. Median total cost for one elderly CAP patient with CVEs was RMB 20,315.5, significantly higher than that (RMB 12,207.1) for non-CVEs patient (p<0.001). All the data are provided in Table 1.
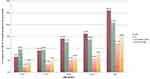
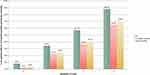
The occurrence of CVEs significantly increased with age (p<0.001), and the incidence in patients aged ≥ 86 years was as high as 25.9%, nearly fourfold than that in patients aged 65–70 years (Figure 1). The rate of CF, in-hospital mortality and 30-day mortality significantly increased with the numbers of CVEs (p<0.001). The rate of in-hospital mortality and 30-day mortality in patients with three types of CVEs was 64.7% and 70.6%, respectively, threefold than that in patients with one type of CVEs and 20–30 folds than that in patients without CVEs (p<0.001) (Figure 2).
Predictive Factors for the Occurrence of CVEs During Hospitalization
Table 3 shows that previous history of CHF (OR 6.16; 95% CI, 4.14–9.18, p<0.001), CF (OR 4.69; 95% CI, 3.392–6.48, p<0.001), previous history of ischemic heart disease (OR 2.22; 95% CI, 1.61–3.07, p<0.001), use of glucocorticoids during hospitalization (OR 2.0; 95% CI, 1.39–2.89, p<0.001), aspiration (OR 1.88; 95% CI, 1.26–2.81, p=0.002), pleural effusion (OR 1.66; 95% CI, 1.25–2.20, p<0.001), multilobe infiltration (OR 1.50; 95% CI, 1.15–1.96, p=0.003), age (OR 1.05; 95% CI, 1.04–1.07, p<0.001), and blood urea nitrogen (BUN) (OR 1.03; 95% CI, 1.01–1.06, p=0.007) were independent predictors for the occurrence of any CVE during hospitalization in the multivariable logistic regression model. While level of blood sodium (OR 0.98; 95% CI, 0.97–0.99, p=0.007) was a protective factor.
 |
Table 3 Predictive Factors for the Occurrence of CVEs During Hospitalization in Univariate and Multivariable Logistic Regression Analysis |
Predictive Factors for 30-Day Mortality in Elderly Patients with CAP
Table 4 shows that renal failure (OR 9.46; 95% CI, 4.17–21.48, p<0.001), respiratory failure (OR 9.32; 95% CI, 5.91–14.71, p<0.001), sepsis/sepsis shock (OR 7.87; 95% CI, 3.58–17.31, p<0.001), new CVDs (OR 5.94; 95% CI, 1.78–19.87, p=0.004), new heart failure (OR 4.04; 95% CI, 1.15–14.14, p=0.029), new arrhythmia (OR 2.38; 95% CI, 1.11–5.14, p=0.027), aspiration (OR 1.95; 95% CI, 1.09–3.50, p=0.025), CURB-65 (OR 1.57; 95% CI, 1.21–2.02, p=0.001), and white blood cell (WBC) count (OR 1.05; 95% CI, 1.02–1.09, p=0.006) were independent predictors for 30-day mortality in elderly patients with CAP in multivariable logistic regression model. While lymphocyte count (OR 0.63; 95% CI, 0.46–0.87, p=0.006) was a protective factor.
 |
Table 4 Predictive Factors for 30-Day Mortality in Elderly CAP Patients in Univariate and Multivariable Logistic Regression Analysis |
Discussion
This is the first retrospective multicenter study to evaluate the disease burden of CVEs and risk factors for incidence of CVEs in hospitalized elderly patients with CAP in China. Our study discovers that: 1) 13.7% of elderly patients with CAP experience CVEs during hospitalization with higher rate of CF and poorer prognosis. 2) Independent risk factors associated with CVEs are age, aspiration, previous history of CHF and ischemic heart disease, level of BUN, CF, use of systematic glucocorticoids during hospitalization, pleural effusion, and multilobe infiltration; while level of blood sodium is a protective factor. 3) Independent risk factors associated with 30-day mortality are renal failure, respiratory failure, sepsis/sepsis shock, new CVDs, new heart failure, new arrhythmia, aspiration, CURB-65, and WBC count; while lymphocyte count is a protective factor.
Nowadays, there were some researches on CVEs during the course of or after CAP. However, the incidence of CVEs differs as the different inclusion criteria of CVEs. In a multicenter prospective study enrolled 1266 patients with CAP, data indicated that 23.8% of patients experienced at least a CV event (excluded the thromboembolic diseases),12 higher than that in our study. We considered the gap is mainly related to the low proportion of patients in PSI class IV or V or CURB-65 class 3–5. The most common CVE during hospitalization is newly diagnosed acute heart failure (11.0%), followed by arrhythmia (3.5%) and AMI (1.1%), similar with the data from systematic review and meta-analysis of observational studies.10 As to the mechanisms about the occurrence of CVEs in patients with CAP, previous studies demonstrated acute or persistent inflammation after CAP became the fuse of potential triggers for cardiac events, leading to the increased pro-inflammatory cytokines or activation of pro-coagulant factors. Plaque-related CVEs (AMI) and plaque-unrelated CVEs (arrhythmias and heart failure) occurred after plaque rupture, in-situ thrombus formation, and alteration of the balance of arterial perfusion or diffuse organ abnormalities with cellular dysfunction.14–18 Additionally, the occurrence of type 2 myocardial infarction (T2MI) after acute infection is considered to be related to“demand ischemia” (a mismatch in myocardial oxygen supply and demand).19 In older adults, coronary stenosis from chronic plaques and possibly toxin-mediated vasoconstriction after acute infection may lead to increased cardiac metabolic mismatch.20 Data discovered T2MI gradually increased with advanced age, especially among patients aged over 75 years old.21 Thence, appropriate antimicrobial regimens, effective treatment against other underlying diseases, anticoagulation therapy, dynamic monitoring of laboratory indicators, and timely adjustment of therapeutic plans can play an important role in the control of inflammation.
The disease burden of elderly patients with CAP experienced CVEs is heavier. In a prospective multicenter cohort of 1182 CAP inpatients enrolled between 2011 and 2016, Francesco Violi et al reported patients who experienced a CVE were older, had a higher prevalence of underlying diseases and complications, higher disease severity, unstable vital signs and 30-day mortality,22 in line with our results. In our study, a significant increasing trend in the proportion of patients with CVEs, CF, and short-term mortality was found across the advanced age; meanwhile, the increased numbers of CVEs lead to poorer prognosis. Patients with CVEs had significantly lower proportion of guideline-concordant antibiotic therapy than that in patients without CVEs, thus, the proportion of CF significantly increased accordingly as well as prolonged LOS and higher short-term mortality.3 This result suggests that appropriated evaluation of pathogens plays an important role in the choice of optimal antimicrobial regimen.
We confirmed previous reports showing that history of heart failure, previously diagnosed coronary artery disease, pleural effusion, multilobe infiltration, age and BUN were independently associated with CVEs.12,16,23–26 In the first analysis of prospectively collected data from the Pneumonia Patient Outcomes Team cohort study in patients with CAP, sodium<130 mmol/L was considered as independent risk factor for incident cardiac complications.25 In our data, level of blood sodium (OR 0.98; 95% CI, 0.97–0.99, p=0.007) was protective factor for the occurrence of CVEs, suggesting the similar conclusion. Adjunctive use of corticosteroids for patients with CAP has been controversial, even for severe CAP.27–29 In a propensity-score adjusted Cox model by Cangemi et al, use of corticosteroid for patients with CAP was associated with a lower incidence of intra-hospital myocardial infarction (OR 0.46; 95% CI 0.24–0.88, p=0.02), albeit not reducing either overall mortality or cardiovascular death.30 Conversely, we found adjunctive use of corticosteroids during hospitalization was associated with a higher incidence of CVEs (OR 2.0; 95% CI, 1.39–2.89, p<0.001). In an observational study of 500 consecutive patients hospitalized with CAP who were enrolled in the Community-Acquired Pneumonia Organization (CAPO) cohort study, data addressed CF was significantly related to the occurrence of AMI (OR, 4.22; 95% CI, 1.10–16.29),31 generally consistent with our conclusion. 21.4% of elderly patients with CVEs in our population had higher risk of aspiration. Aspiration can bring about chemical pneumonia, bacterial pneumonia, or lipoid pneumonia, and thus lead to acute or chronic infection and inflammation. Acute infections not only destabilize vascular endothelium and result in an imbalance between myocardial oxygen supply and demand, but also have both systemic and local effects on coronary vessels, thence creating an increased risk of cardiovascular events.32,33 In our multivariable logistic regression analysis, aspiration was confirmed as an independent predictor for CVEs.
The results of the current study are concordant with previous evidence that aspiration, CURB-65, WBC count, sepsis/sepsis shock and respiratory failure were independent predictors for short-term mortality for elderly patients with CAP.4,34–37 We found the complication after CAP, renal failure was significantly associated with increased 30-day mortality (OR 9.46; 95% CI, 4.17–21.48, p<0.001). Yet, in the past literatures, BUN is more used to an evaluation indicator. A retrospective cohort study from China by Kang and coworkers assessing 4880 CAP patients aged ≥ 65 years showed that BUN was a prognostic factor for in-hospital mortality.35 Data from a multicenter prospective study on the Implications of acute Cardiovascular Events in patients hospitalized for Community-Acquired Pneumonia (ICECAP), enrolling patients consecutively hospitalized from 2016 to 2018, indicated the occurrence of any CVE during hospitalization independently and significantly increased the risk of 30-day mortality (HR 1.69; 95% CI, 1.14–2.51, p = 0.009); while newly diagnosed heart failure, new onset atrial fibrillation or flutter, acute coronary syndrome, separately, were not associated with increased risk of 30-day mortality.12 The current study is the first to our knowledge to illustrate new CVDs, new heart failure, and new arrhythmia were independently and significantly increased the risk of 30-day mortality for elderly patients with CAP.
There are some limitations in our study that should be acknowledged. The present study was a retrospective design; thus, missing data were inevitable There were no records about the timing of onset of CVEs, the detailed type of new arrhythmia and CVDs during hospitalization. Furthermore, medications like statins and anticoagulants during hospitalization were also not evaluated. Meanwhile, we did not evaluate the association between pathogens or antimicrobial treatment and the occurrence of CVEs. Finally, biomarkers such as D-dimer, BNP, NT-proBNP presented lots of missing values, thereby, the relationship between biomarkers and the occurrence of CVEs could not be explored.
Conclusions
CVEs during hospitalization are common in elderly patients with CAP in China. Patients with CVEs have heavier disease burden and poorer outcomes, especially those with new CVDs, new heart failure, and new arrhythmia, which are independently and significantly prognostic factors for short-term mortality. It is critical for clinicians to early identify risk factors and strengthen the hierarchical management of elderly patients with CAP.
Abbreviations
CVEs, cardiovascular events; CAP, community-acquired pneumonia; CHF, congestive heart failure; CVDs, cerebrovascular diseases; CF, clinical failure; OR, odds ratio; ICU, intensive care unit; WHO, World Health Organization; LOS, length of stay; BNP, brain natriuretic peptide; NT-proBNP, N-terminal pro-B-type natriuretic peptide; AMI, acute myocardial infarction; PE, pulmonary embolism; DVT, deep venous thrombosis; IQR, interquartile range; CIs, confidence intervals; DIC, diffuse intravascular coagulation; BUN, blood urea nitrogen; WBC, white blood cell; PSI, pneumonia severity index; T2MI, type 2 myocardial infarction; CAPO, Community-Acquired Pneumonia Organization; ICECAP, Implications of acute Cardiovascular Events in patients hospitalized for Community-Acquired Pneumonia; DIC, disseminated intravascular coagulation; COPD, chronic obstructive pulmonary disease; HCAP, healthcare-associated pneumonia; RR, respiratory rate; HR, heart rate; HCT, hematocrit; Cr, creatinine; Na, sodium; PaO2/FiO2, partial arterial oxygen pressure/fraction of inspired oxygen; PaO2, partial arterial oxygen pressure; SaO2, arterial oxygen saturation; CT, computed tomography.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Ethics Approval and Informed Consent
This study was approved by the China-Japan Friendship Hospital Ethics Committee (No. 2015–85) on October 12, 2015. We also confirmed that all patient data was treated with confidentiality, in accordance with the Declaration of Helsinki.
Consent for Publication
All authors have confirmed that the details of the paper.
Acknowledgments
The authors are grateful for the contributions of all the staff of the CAP-China network for their help with data collection and input. Thanks to Yimin Wang, Guangqiang Wang, Xuexin Yao, Hongxia Yu, Guohua Yu, Meng Liu, Chunxue Xue, Bo Liu, Xiaoli Zhu, Yanli Li, Ying Xiao, Xiaojing Cui, Lijuan Li, and Lei Wang for collecting the information. Thanks to Yi Wang for revising the figures.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Science Grant for Distinguished Young Scholars (grant number 81425001/H0104), the National Key Technology Support Program from Ministry of Science and Technology (grant number 2015BAI12B11) and the Beijing Science and Technology Project (grant number D151100002115004).
Disclosure
The authors declare that they have no competing interests.
References
1. Ferreira-Coimbra J, Sarda C, Rello J. Burden of community-acquired pneumonia and unmet clinical needs. Adv Ther. 2020;37(4):1302–1318. doi:10.1007/s12325-020-01248-7
2. Cillóniz C, Dominedò C, Pericàs JM, Rodriguez-Hurtado D, Torres A. Community-acquired pneumonia in critically ill very old patients: a growing problem. Eur Respir Rev. 2020;29(155):190126. doi:10.1183/16000617.0126-2019
3. Han X, Liu X, Chen L, et al. Disease burden and prognostic factors for clinical failure in elderly community acquired pneumonia patients. BMC Infect Dis. 2020;20(1):668. doi:10.1186/s12879-020-05362-3
4. Han X, Zhou F, Li H, et al. Effects of age, comorbidity and adherence to current antimicrobial guidelines on mortality in hospitalized elderly patients with community-acquired pneumonia. BMC Infect Dis. 2018;18(1):192. doi:10.1186/s12879-018-3098-5
5. Furman CD, Leinenbach A, Usher R, Elikkottil J, Arnold FW. Pneumonia in older adults. Curr Opin Infect Dis. 2021;34(2):135–141. doi:10.1097/QCO.0000000000000718
6. World Health Organization. The top 10 causes of death. Avialable from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
7. Lopez-Otin C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153:1194–1217. doi:10.1016/j.cell.2013.05.039
8. Corrales-Medina VF, Alvarez KN, Weissfeld LA, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA. 2015;313:264–274. doi:10.1001/jama.2014.18229
9. Corrales-Medina VF, Taljaard M, Fine MJ, et al. Risk stratification for cardiac complications in patients hospitalized for community-acquired pneumonia. Mayo Clin Proc. 2014;89(1):60–68. doi:10.1016/j.mayocp.2013.09.015
10. Tralhão A, Póvoa P. Cardiovascular events after community‐acquired pneumonia: a global perspective with systematic review and meta‐analysis of observational studies. J Clin Med. 2020;9(2):414. doi:10.3390/jcm9020414
11. Chen L, Han X, Li Y, Zhang C, Xing X. Complications of cardiovascular events in patients hospitalized with influenza-related pneumonia. Infect Drug Resist. 2021;14:1363–1373. doi:10.2147/IDR.S305509
12. Pieralli F, Vannucchi V, Nozzoli C, et al. Acute cardiovascular events in patients with community acquired pneumonia: results from the observational prospective FADOI-ICECAP study. BMC Infect Dis. 2021;21(1):116. doi:10.1186/s12879-021-05781-w
13. Putot A, Bouhey E, Tetu J, et al. Troponin elevation in older patients with acute pneumonia: frequency and prognostic value. J Clin Med. 2020;9(11):3623. doi:10.3390/jcm9113623
14. Ross R, Epstein FH. Atherosclerosis – an inflammatory disease. N Engl J Med. 1999;340:115–126. doi:10.1056/NEJM199901143400207
15. Corrales-Medina VF, Madjid M, Musher DM. Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis. 2010;10:83–92. doi:10.1016/S1473-3099(09)70331-7
16. Aliberti S, Ramirez JA. Cardiac diseases complicating community-acquired pneumonia. Curr Opin Infect Dis. 2014;27(3):295–301. doi:10.1097/QCO.0000000000000055
17. Violi F, Carnevale R, Calvieri C, et al. Nox2 up-regulation is associated with an enhanced risk of atrial fibrillation in patients with pneumonia. Thorax. 2015;70:961–966. doi:10.1136/thoraxjnl-2015-207178
18. Rae N, Finch S, Chalmers JD. Cardiovascular disease as complication of community-acquired pneumonia. Curr Opin Pulm Med. 2016;22(3):212–218. doi:10.1097/MCP.0000000000000261
19. Musher DM, Abers MS, Corrales-Medina VF, Longo DL. Acute Infection and Myocardial Infarction. N Engl J Med. 2019;380(2):171–176. doi:10.1056/NEJMra1808137
20. Sibelius U, Grandel U, Buerke M, et al. Staphylococcal alpha-toxin provokes coronary vasoconstriction and loss in myocardial contractility in perfused rat hearts: role of thromboxane generation. Circulation. 2000;101(1):78–85. doi:10.1161/01.CIR.101.1.78
21. Putot A, Chague F, Manckoundia P, Cottin Y, Zeller M. Post-infectious myocardial infarction: new insights for improved screening. J Clin Med. 2019;8(6):827. doi:10.3390/jcm8060827
22. Violi F, Cangemi R, Falcone M, et al. Cardiovascular complications and short-term mortality risk in community-acquired pneumonia. Clin Infect Dis. 2017;64(11):1486–1493. doi:10.1093/cid/cix164
23. Aliberti S, Ramirez J, Cosentini R, et al. Acute myocardial infarction versus other cardiovascular events in community-acquired pneumonia. ERJ Open Res. 2015;1(1):00020–2015. doi:10.1183/23120541.00020-2015
24. Cangemi R, Calvieri C, Falcone M, et al. Relation of cardiac complications in the early phase of community-acquired pneumonia to long-term mortality and cardiovascular events. Am J Cardiol. 2015;116(4):647–651. doi:10.1016/j.amjcard.2015.05.028
25. Corrales-Medina VF, Musher DM, Wells GA, Chirinos JA, Chen L, Fine MJ. Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality. Circulation. 2012;125(6):773–781. doi:10.1161/CIRCULATIONAHA.111.040766
26. Viasus D, Garcia-Vidal C, Manresa F, Dorca J, Gudiol F, Carratalà J. Risk stratification and prognosis of acute cardiac events in hospitalized adults with community acquired pneumonia. J Infect. 2013;66(1):27–33. doi:10.1016/j.jinf.2012.09.003
27. Medical Letter on Drugs and Therapeutics. Corticosteroids in Community-Acquired Pneumonia. JAMA. 2020;323(9):887–888. doi:10.1001/jama.2020.0216
28. Jiang S, Liu T, Hu Y, et al. Efficacy and safety of glucocorticoids in the treatment of severe community-acquired pneumonia: a meta-analysis. Medicine. 2019;98(26):e16239. doi:10.1097/MD.0000000000016239
29. Torres A, Sibila O, Ferrer M, et al. Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: a randomized clinical trial. JAMA. 2015;313(7):677–686. doi:10.1001/jama.2015.88
30. Cangemi R, Falcone M, Taliani G, et al. Corticosteroid use and incident myocardial infarction in adults hospitalized for community‐acquired pneumonia. Ann Am Thorac Soc. 2019;16(1):91–98. doi:10.1513/AnnalsATS.201806-419OC
31. Ramirez J, Aliberti S, Mirsaeidi M, et al. Acute myocardial infarction in hospitalized patients with community-acquired pneumonia. Clin Infect Dis. 2008;47(2):182–187. doi:10.1086/589246
32. Petroianni A, Ceccarelli D, Conti V, Terzano C. Aspiration pneumonia. Pathophysiological aspects, prevention and management. A review. Panminerva Med. 2006;48(4):231–239.
33. Singanayagam A, Singanayagam A, Elder DH, Chalmers JD. Is community-acquired pneumonia an independent risk factor for cardiovascular disease? Eur Respir J. 2012;39(1):187–196. doi:10.1183/09031936.00049111
34. Feng DY, Zou XL, Zhou YQ, Wu WB, Yang HL, Zhang TT. Combined neutrophil-to-lymphocyte ratio and CURB-65 score as an accurate predictor of mortality for community-acquired pneumonia in the elderly. Int J Gen Med. 2021;14:1133–1139. doi:10.2147/IJGM.S300776
35. Kang Y, Fang XY, Wang D, Wang XJ. Activity of daily living upon admission is an independent predictor of in-hospital mortality in older patients with community acquired pneumonia. BMC Infect Dis. 2021;21(1):314. doi:10.1186/s12879-021-06006-w
36. Yoshikawa H, Komiya K, Yamamoto T, et al. Quantitative assessment of erector spinae muscles and prognosis in elderly patients with pneumonia. Sci Rep. 2021;11(1):4319. doi:10.1038/s41598-021-83995-3
37. Leroy O, Bosquet C, Vandenbussche C, et al. Community-acquired pneumonia in the intensive care unit: epidemiological and prognosis data in older people. J Am Geriatr Soc. 1999;47(5):539–546. doi:10.1111/j.1532-5415.1999.tb02567.x