Source/Disclosures
Published by:
Naqash AR, et al. Abstract 2508. Presented at: ASCO Annual Meeting; June 3-7, 2022; Chicago.
Disclosures:
NIH funded this study. Naqash reports no relevant disclosures. Please see the abstract for all other researchers’ relevant financial disclosures.
CHICAGO — Patients and prescribers should be more aware of the potential for major adverse cardiac events after immune checkpoint inhibitor-based therapy, according to retrospective study results presented at ASCO Annual Meeting.
The association between immune major adverse cardiac events (MACE) and noncardiac immune-related adverse events highlights the importance of a multidisciplinary management approach, researchers emphasized.

Data derived from Naqash AR, et al. Abstract 2508. Presented at: ASCO Annual Meeting; June 3-7, 2022; Chicago.
“To the best of our knowledge, this is the first-ever pooled analysis of immune checkpoint inhibitor clinical trials evaluating major adverse cardiac events,” Abdul Rafeh Naqash, MD, assistant professor in the early phase division of Stephenson Cancer Center at University of Oklahoma, said during a presentation. “These findings have important management implications, as more and more patients are being treated with anti-pD-1/PD-l1 combinations.”
Background and methods
Although rare, MACE can manifest in various ways among patients treated with immune checkpoint inhibitors. These events can result in considerable morbidity or death.
More work is needed to better define presentation of these events and their potential relationship with noncardiac immune-related adverse events among patients treated with immune checkpoint inhibitors, according to study background.

Abdul Rafeh Naqash
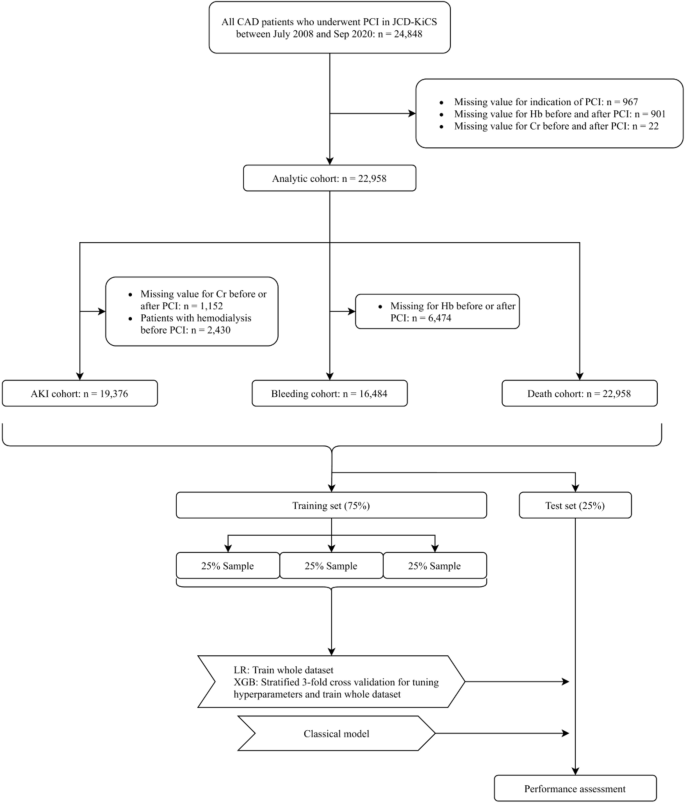
Naqash and colleagues performed a retrospective pooled analysis of MACE captured in the NCI-Cancer Therapy Evaluation Program’s serious adverse events reporting database.
The analysis included patients treated with anti-PD-1/-PD-L1 therapy alone or in combination with other anticancer therapies as part of NCI-sponsored investigational clinical trials in the United States and Canada between June 2015 and December 2019.
The analysis included 6,925 patients. Slightly less than half (48%) received single-agent anti-PD-1/PD-L1 therapy. The remainder received those agents as part of combination therapy.
Results
Forty patients (0.6%; median age, 68.5 years; 60% men) developed immune checkpoint inhibitor-related MACE.
The most common malignancies in this group included melanoma (37.5%), genitourinary cancer (16%), gastrointestinal cancer (12.5%), gynecologic cancer (7.5%), lymphoma (5%) and lung cancer (5%).
Median time to MACE from initial immune checkpoint inhibitor administration was approximately 28 days.
Researchers characterized the majority (77.5%) of MACE as grade 3 or higher (grade 3, 50%; grade 4, 20%; grade 5, 7.5%).
Myocarditis accounted for nearly half (45%; n = 18) of MACE, occurring a median two doses after immune checkpoint inhibitor administration. The majority (78%) of cases were grade 3 or higher.
Seventy-two percent of patients with myocarditis had been treated with anti-PD-1/PD-L1-based combination regimens, the most common of which included an anti-CTLA-4 inhibitor (92%).
Researchers reported four myocarditis-related deaths. All four of these individuals had concurrent myositis and three had concurrent transaminitis.
Nonmyocarditis MACE included dysrhythmias, cardiomyopathy, pericardial disorders, acute coronary syndrome and cardiac arrest.
More than half (65%) of patients who developed MACE experienced multisystem organ involvement with other noncardiac immune-related adverse events, the two most common being myositis (27.5%) and transaminitis (25%).
Nearly all patients (92.5%) with MACE required hospitalization and 30% required ICU admission.
Most patients (83%) with myocarditis experienced at least one noncardiac immune-related adverse event, and 50% of those with non-myocarditis MACE developed noncardiac immune-related adverse events.
Forty percent of those who developed MACE received single-agent PD-1/PD-L1 agent therapy, and 60% had received anti-PD-1/PD-L1 in combination with other therapies.
MACE occurred more frequently among patients treated with anti-PD-1/PD-L1 plus targeted therapies (2.1%) than anti-PD-1/PD-L1 plus anti-CTLA-4 therapies (0.9%), anti-PD-1/PD-L1 plus chemotherapy (0.83%) or single-agent anti-PD-1/PD-L1 (0.47%).
Next steps
Immune checkpoint inhibitor-related MACE has heterogeneous presentation and often is associated with poor prognosis, Naqash said.
“This makes timely identification and intervention critical,” Naqash said. “We also saw complex noncardiac immune-related adverse events present concurrently, which makes incorporation of a multidisciplinary approach consisting of cardiologists, oncologists, internists and other subspecialists essential in the management of these patients. In addition, the type of combination therapy may influence MACE risk and incidence, which suggests better characterization of MACE with anti-PD-1/PD-L1-based combination therapies is required.”