March 15, 2022
3 min read
Source/Disclosures
Published by:
Disclosures:
Paterson reports no relevant financial disclosures. Please see the study for all other authors’ relevant disclosures. Ohtsu and colleagues report no relevant financial disclosures.
New cancer diagnosis appeared associated with increased risk for cardiovascular death, as well as incident heart failure, stroke or pulmonary embolism, according to a retrospective cohort study published in JACC: CardioOncology.
“This risk persisted to at least 7 years from cancer diagnosis and appeared most pronounced in patients with hematologic, gastrointestinal, genitourinary and thoracic malignancies,” D. Ian Paterson, MD, FRCPC, professor of medicine in the division of cardiology, director of the Edmonton Cardio-Oncology Program and director of academic and research cardiac MRI at University of Alberta, told Healio.
Background and methodology
Paterson and colleagues pursued the research because, despite the knowledge that patients with cancer and cancer survivors are at increased risk for heart failure, previous data conflicted regarding long-term risk for other cardiovascular events, as well as risk according to cancer site.
“Population studies to date have largely evaluated the risk [for] cardiovascular disease — and usually only heart failure — in patients with breast cancer,” Paterson said. “We performed a comprehensive analysis of the risk [for] incident cardiovascular disease in patients with a new cancer diagnosis of any type.”

D. Ian Paterson
The analysis included 4,519,243 adults who resided in Alberta, Canada, from April 2007 to December 2018. Among them, 224,016 (median age, 56 years; range, 43-67; 56.8% women) had a new cancer diagnosis and 4,295,227 (median age, 34 years; range, 23-49; 48.5% women) comprised the control population.
Paterson and colleagues used time-to-event survival models, after adjusting for comorbidities and sociodemographic factors, to compare the two cohorts with respect to risk for subsequent cardiovascular events, which included cardiovascular mortality, myocardial infarction, stroke, heart failure and pulmonary embolism.
Determining the impact of new cancer diagnosis on risk for fatal and nonfatal cardiovascular events served as the primary outcome.
Key findings
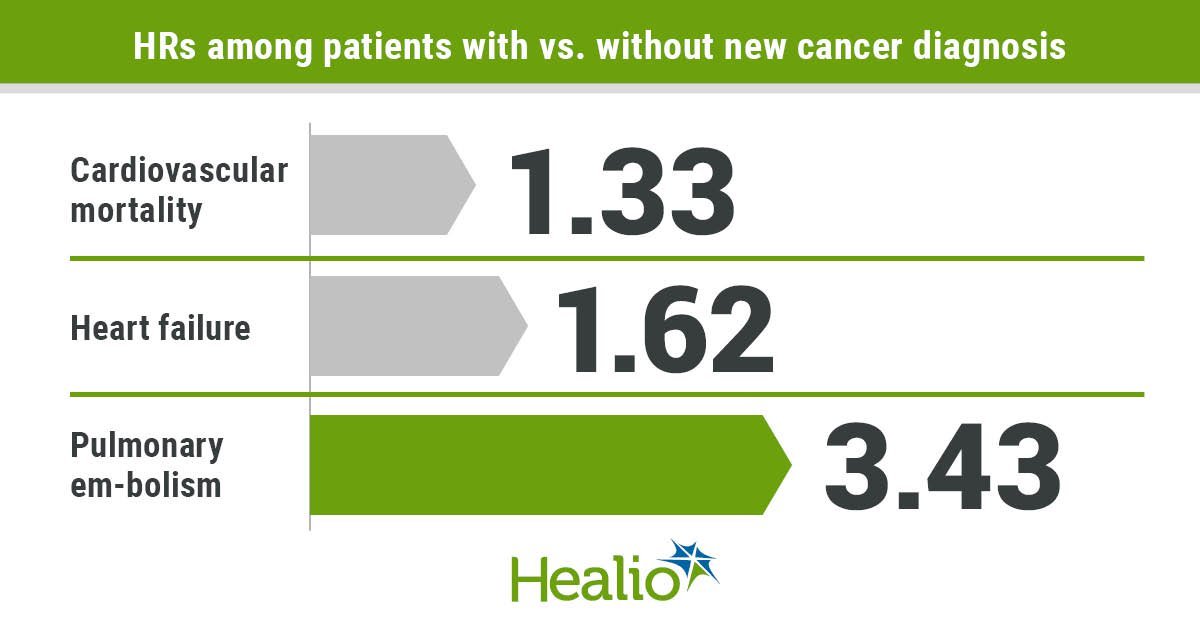
At median follow-up of 11.8 years, results showed 73,360 cardiovascular deaths and 470,481 nonfatal cardiovascular events. After adjustment, researchers reported participants with cancer demonstrated the following HRs compared with participants without cancer:
1.33 (95% CI, 1.29-1.37) for cardiovascular mortality;
1.01 (95% CI, 0.97-1.05) for myocardial infarction;
1.44 (95% CI, 1.41-1.47) for stroke;
1.62 (95% CI, 1.59-1.65) for heart failure; and
3.43 (95% CI, 3.37-3.5) for pulmonary embolism.
Additionally, patients with genitourinary, gastrointestinal, thoracic, neurologic and hematologic malignancies demonstrated the highest cardiovascular risk.
“We were surprised that the risk [for] incident cardiovascular disease remained elevated in patients with cancer, even after fully adjusted risk modeling,” Paterson told Healio. “This suggests that the cancer itself, cancer therapies and/or other less traditional risk factors, such as physical activity and body composition, may have also contributed to cardiovascular risk.”
Implications
Paterson and colleagues wrote that future studies should investigate other potential contributors to cardiovascular risk, including cancer therapies and emerging risk factors for cardiotoxicity.
“We would like to identify effective intervention strategies to mitigate cardiovascular risk in patients with cancer, especially in the higher-risk cancer types (eg, hematologic),” Paterson said.
Paterson noted that as life expectancy of patients with cancer increases, so does their likelihood of developing other illnesses after diagnosis, necessitating a more collaborative approach to their health care. The authors of a corresponding editorial concurred.
“Perhaps the lesson we need to learn from [this study] is that it is time for cardiology and oncology to collaborate in order to travel upstream and build a powerhouse to generate information from the new flow of data efficiently,” Hiroshi Ohtsu, MS, manager of clinical epidemiology and director of JCRAC data center at National Center for Global Health and Medicine, Center for Clinical Sciences in Japan, and colleagues wrote.
“Cardiology and oncology need to collaborate to launch and successfully execute projects to establish new techniques to use real-world data for real-world evidence,” they added.
Reference s :
For more information:
D. Ian Paterson, MD, FRCPC, can be reached at Division of Cardiology, University of Alberta, 8440 112 St., 2C2.43 WCM, Edmonton, Alberta T6G2B7, Canada; email: ip3@ualberta.ca.





